How Age Affects Fertility in Women
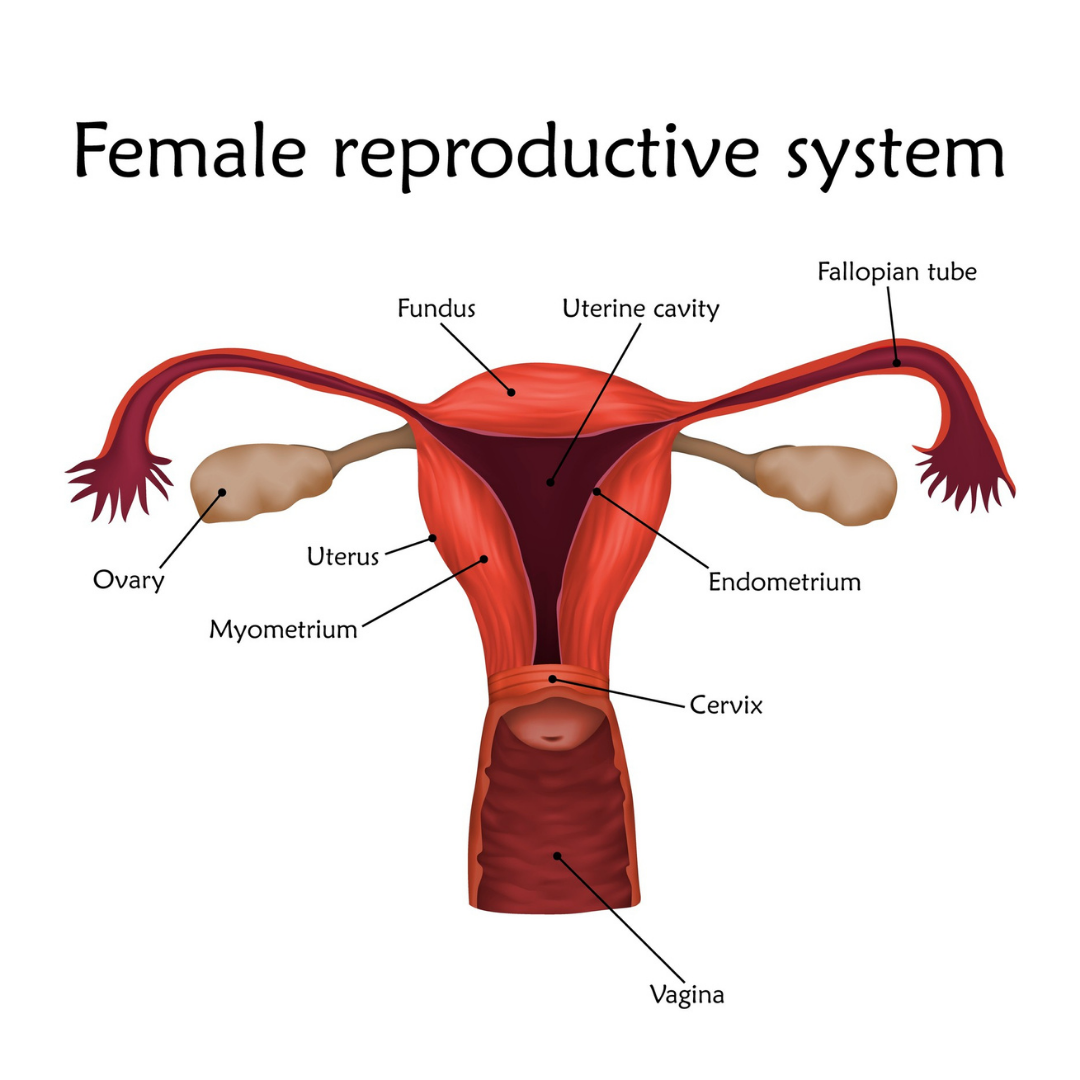
Although women are born with millions of eggs in their ovaries, only a few hundred reach maturity and are ovulated over the course of the lifetime.
Women are born with all of their eggs in their ovaries, but only start to release eggs for fertilization during puberty.
Egg Quantity & Quality
As women age, the number of eggs decreases. The quality of these eggs also decreases, making it more difficult to become pregnant and increasing the chances of miscarriage. A woman’s fertility is constantly declining from birth but starts to change more abruptly in the mid-30s.
Menopause & Perimenopause
Menopause is defined as no period for a year in the setting of low egg supply. The average age of menopause is 50, but the quality and reproductive potential of eggs sharply decrease 8-10 years before menopause.
In the time frame before menopause, often referred to as perimenopause, women will have a reduction of their egg quality and quantity. They may experience shorter menstrual cycles leading to missing periods. After menopause, women can no longer become pregnant using their own eggs. However, with the use of third party reproduction including donor egg or donor embryo, menopausal women are able to carry a pregnancy.