Who Can Benefit from In Vitro Fertilization?
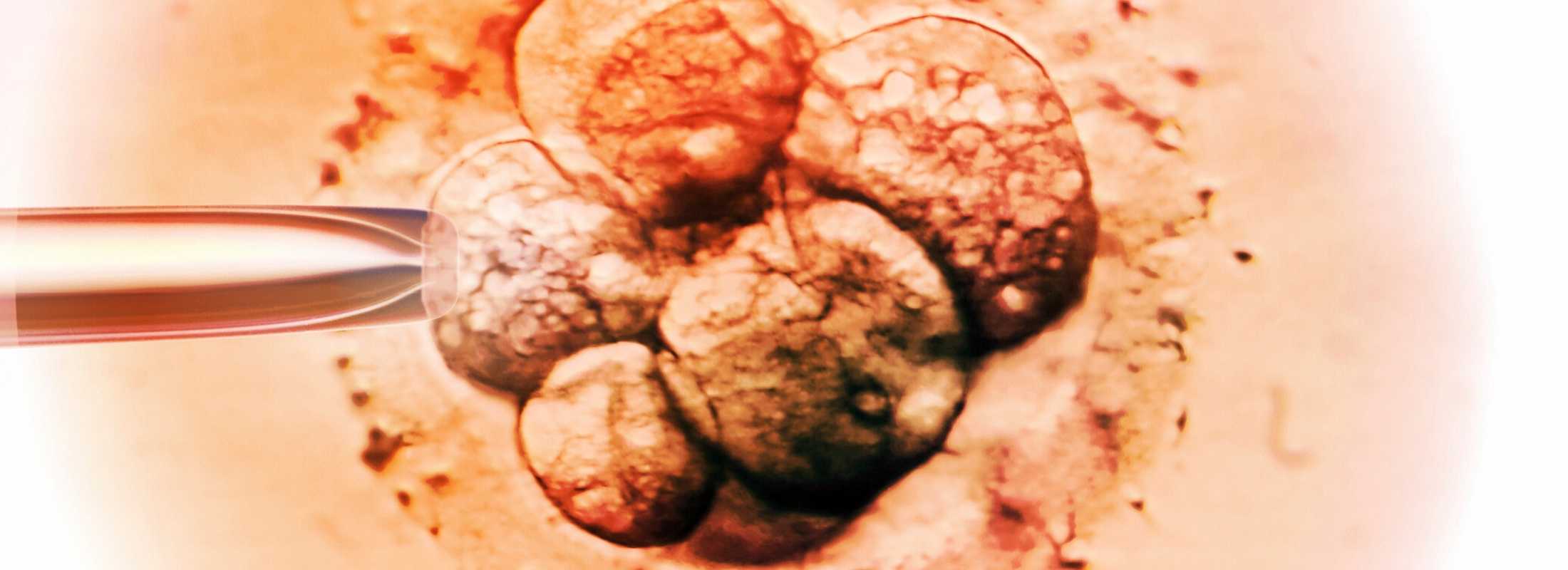
IVF is often not the initial recommended treatment but could be the first step for those who have absent or nonfunctional fallopian tubes and if the sperm quality is very poor. IVF used to treat infertility is also a good option for those wishing to have a large family, due to the prospect of multiple frozen embryos.
In vitro fertilization is also used for potential fertility preservation, in collecting and freezing sperm or eggs for later pregnancy, either due to individual preferences or an upcoming medical treatment such as fertility harming chemotherapy.
We always evaluate people who come to us for infertility solutions with an eye toward using the least invasive treatments when possible. These can be as simple as lifestyle changes or medications.
In many cases, other infertility treatments such as intrauterine insemination (IUI) should be considered before IVF. If these are not successful, IVF is often the next step.
IVF can help those with issues such as:
- Endometriosis
- Fallopian tube or uterine abnormalities
- Poor quality sperm
- Ovulation disorders
- Unexplained infertility
- Recurrent miscarriage
Additionally, in vitro fertilization can help those who otherwise could not experience pregnancy and/or parenthood biologically. This includes patients who need donor eggs or another individual to carry the pregnancy (a gestational carrier, also known as a surrogate) to build their family.