16 Oct Unraveling the Connection: Should I remove my IUD?
We are exploring a question often posed by our patients: “Should I remove my IUD (Intrauterine devices) to freeze embryos or eggs for the future?” We will provide evidence-based insights and expert opinions to guide you through this aspect of your fertility journey.
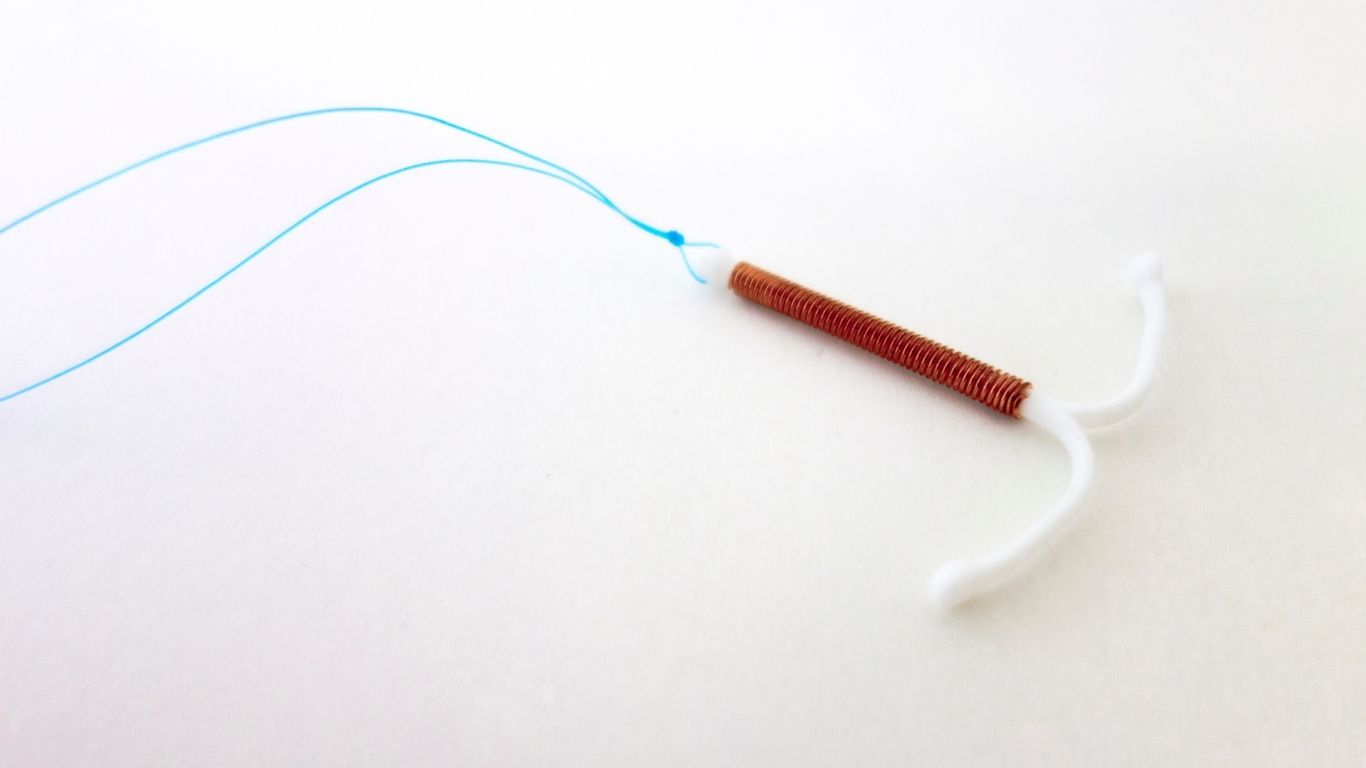
Decoding IUDs
Intrauterine devices (IUDs), either hormonal or copper, are valued for their effectiveness as contraceptives. According to the American College of Obstetricians and Gynecologists, IUDs are over 99% effective at preventing pregnancy (ACOG, 2019).
Looking to get pregnant now or near future
If you are looking to move forward with assisted reproductive technologies (ART) like IVF with the hopes of building your family now, then the removal of your IUD is required. Once embryos have been created, the embryo is placed inside of the uterus – thus, an IUD would prevent implantation of an embryo.
If you are freezing eggs or embryos for the future
Then, you most likely do NOT need to remove IUD. This process involves ovarian stimulation (with gonadotropin injections) followed by the extraction of eggs directly from the ovaries. Let us make a list of pros and cons.
Pros:
- No need to remove and replace IUD. Eliminates cost, discomfort, multiple doctor visits.
- difference in the number of mature eggs retrieved with IUD vs no IUD in several studies.
- Once decide to use those eggs in the future, there is no difference in pregnancy rates or live birth rates when eggs were collected while IUD was in place.
Cons:
- The amount of gonadotropins required is higher on average per cycle, which can increase cost. However, in one study, the absolute difference was just over 200 units of drug (which is equivalent to around ~$200 of added cost).
A Personalized Approach at FSMG
At FSMG, every patient’s journey is distinct. Dr. Morales emphasizes, “We adhere to a personalized approach, meticulously evaluating individual health profiles, contraceptive methods, and overall reproductive health to align our treatments with each patient’s unique needs and aspirations.”
Embarking on the fertility pathway requires nuanced decision-making. Our dedicated team at FSMG is committed to walking alongside you, offering expertise, care, and support tailored just for you.
Request an appointment: CLICK HERE
References:
- American College of Obstetricians and Gynecologists (ACOG). (2019). Long-Acting Reversible Contraception (LARC): IUD and Implant. Retrieved from [ACOG website](https://www.acog.org/patient-resources/faqs/contraception/long-acting-reversible-contraception-iud-and-implant)
- American Society for Reproductive Medicine (ASRM). (2014). Mature Oocyte Cryopreservation: A Guideline. Fertility and Sterility, 101(2), 376-383. Retrieved from [ASRM website](https://www.asrm.org/globalassets/asrm/asrm-content/news-and-publications/practice-guidelines/for-non-members/mature_oocyte_cryopreservation10.13.pdf)
- Amanda J. Adeleye, Lusine Aghajanova, Chia-Ning Kao, Marcelle I. Cedars, Mark V. Sauer,Impact of the levonorgestrel-releasing intrauterine device on controlled ovarian stimulation outcomes,Fertility and Sterility,Volume 110, Issue 1,2018,Pages 83-88, ISSN 0015-0282,https://doi.org/10.1016/j.fertnstert.2018.03.022.


